An In-Shoe Journey to Offload a Patient with Charcot Foot Deformity
 David Sutton, Certified Pedorthist & Clinical Advisor
David Sutton, Certified Pedorthist & Clinical Advisor
The following case study was provided by David Sutton, a certified Pedorthist and clinical advisor.
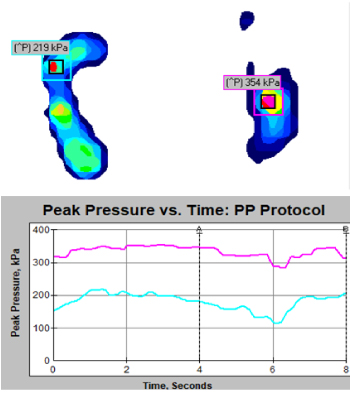 Fig #1: Pressure mat measurement using bilateral loading. Notice the wavering PP; highly unstable.
Fig #1: Pressure mat measurement using bilateral loading. Notice the wavering PP; highly unstable.
Off-loading a Charcot foot deformity and a fused ankle can make for a real challenge, not just because of the changed function but, also the altered shape of the foot and the history of ulcers.
These patients commonly suffer from anxiety and depression, and often lower than average muscle strength. All together, this means their gait is not a fluid like motion, their feet tend to fall to the ground and swing forward rather than moved forward in a meaningful and purposeful way. Improving their self-esteem, motivation and reduce their risk of falls, can improve compliance and assist in reduction of possible further ulceration.
With all of that in mind, we need to create footwear that works well, is easy to don and looks good, because if we can’t do that, compliance will be low and we will have failed.
We use in-shoe pressure mapping to ensure we have the PP (peak pressure) down to the 200kPa (Schaper et al. 2019) and (van Netten et al. 2017). The data produced is great for showing patients their real-time outcomes. Often patients don’t feel anything different or the benefits, but if we show them the data to support our treatment, they are often stunned at both the outcome, and the effort that has been put in to achieve the goal.
On our initial appointment we took a measure of pressure distribution, to gather a baseline, using a pressure mat (see Fig #1) normally we would take and in-shoe measurement, but due to the fact he was wearing a CAM boot on one foot and a slipper on the other; it didn’t seem relevant. From that, viewing his X-rays and a clinical assessment of ROM (range of motion) the decision was made to create custom footwear and foot-orthoses.
Once a LASER scan of the feet was taken (see Fig #2) we created a custom made last. From the last we create a clear check fit to ensure the footwear will fit, and to further engage the patient in the outcome; providing a visual representation of the footwear shape, and how well the client will fit into the footwear.
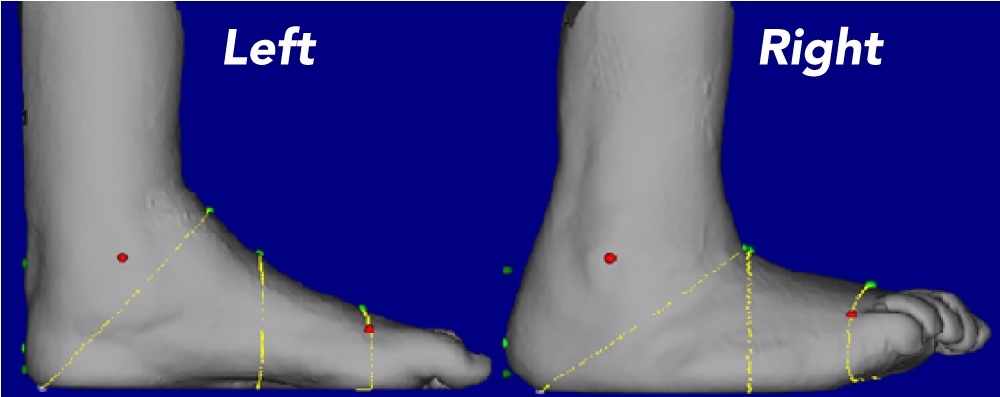 Fig #2: 3D LASER scan of the feet for Last making in a static moment. Visible deformity in the right foot and the inclined ankle, combined with the PP from the Mat is sufficient evidence to support that this patient will fail in a prefab shoe; client has a history of failure in prefabricated footwear.
Fig #2: 3D LASER scan of the feet for Last making in a static moment. Visible deformity in the right foot and the inclined ankle, combined with the PP from the Mat is sufficient evidence to support that this patient will fail in a prefab shoe; client has a history of failure in prefabricated footwear.
Once the ankle boot and orthoses are made, we can begin the in-shoe pressure mapping journey.
We collect data from an 8-step average which the software places a mask over the highest PP (Peak Pressure) area; bilaterally. After the first in-shoe assessment (see Fig #3) in the new custom footwear and orthoses, we modified the right boot in reference to the data collected; 5mm in thickness was added to the sole, for the left we moved the sole fulcrum more proximal and added a met dome to the left orthosis, the results can be seen on the 2nd in-shoe pressure mapping assessment (see Fig #4).
An LLD (leg length discrepancy) is often over looked, and even more so the contralateral limb can be neglected, but as little as a 5mm LLD can make a considerable difference to both feet. Adding 5mm to the right boot decreased PP loading of 335kPa > 149kPa under the base of the 5th MPJ of the right foot, but this action also changed the loading of the left heel (see Fig #4).
After the second assessment, we again modified the left sole fulcrum, moving it further proximal and increased the met dome on the left orthosis. No further modification has been made to both right devices, but there was a slight change in the loading (see Fig #5). After that third assessment, the client was sent home with strict wearing instructions; it is not uncommon for patients to want to wear the new boots and do twice as much as they would normally and this needs to be moderated and controlled to ensure a good long-term outcome for the patient.
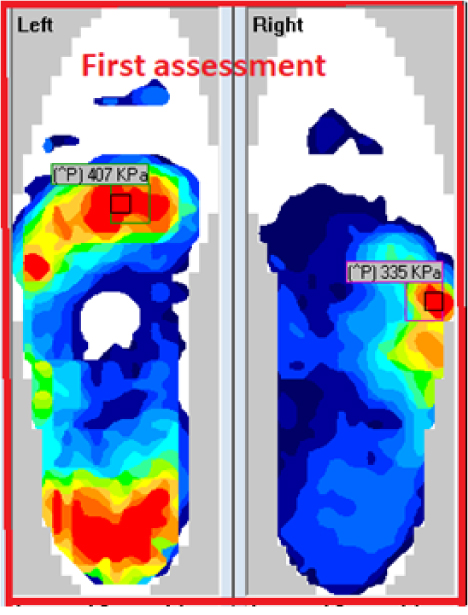 Fig #3: First F-Scan assessment Fig #3: First F-Scan assessment
|
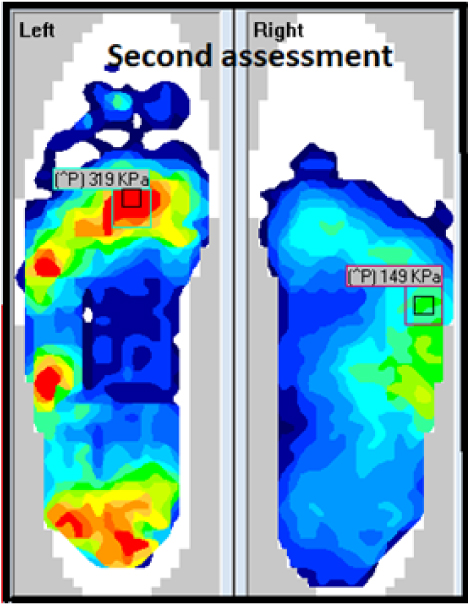 Fig #4: Second F-Scan assessment. Fig #4: Second F-Scan assessment.
|
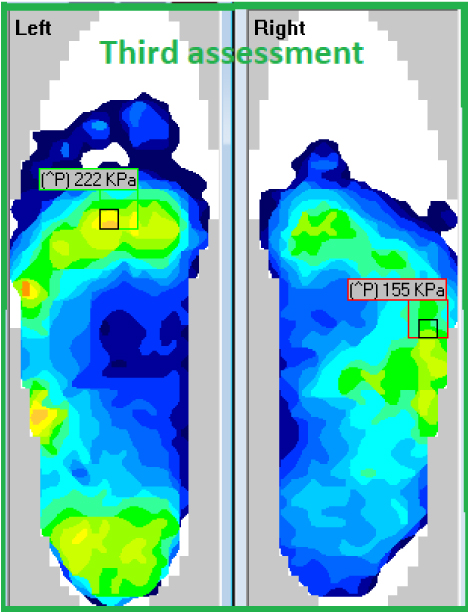 Fig #5: Third F-Scan assessment, and the final outcome for the patient. Fig #5: Third F-Scan assessment, and the final outcome for the patient.
|
References:
Schaper, N. C., van Netten, J. J., Apelqvist, J., Bus, S. A., Hinchliffe, R. J., Lipsky, B. A., & IWGDF Editorial Board. (2020). Practical Guidelines on the prevention and management of diabetic foot disease (IWGDF 2019 update). Diabetes/Metabolism Research and Reviews, 36, e3266.
van Netten, J. J., Lazzarini, P. A., Fitridge, R., Kinnear, E. M., Griffiths, I., Malone, M., Perrin, B., Prentice, J., Sethi, S., & Wraight, P. R. (2017). Australian diabetes-related foot disease strategy 2018-2022: the first step towards ending avoidable amputations within a generation.
More from David Sutton
In this webinar, David shares a case study on his strategy for offloading a patient suffering from a four-year reoccurring diabetic ulcer, using F-Scan as a critical method to verify his decisions.

